Loop Electrosurgical Excision Procedure (LEEP)
LEEP is a widely utilized treatment method for excising abnormal cervical tissue.
What is Cervical Dysplasia?
Cervical dysplasia refers to abnormal changes or growths in the cells of the cervix, the lower part of the uterus that connects to the vagina. These abnormalities can be identified through cervical cytology (Pap smear) or cervical biopsy.
Cervical dysplasia is often associated with infection by the Human Papillomavirus (HPV), a common sexually transmitted virus known to cause cellular changes in the cervix. The severity of cervical dysplasia correlates with the degree of cellular changes: mild to moderate dysplasia may resolve spontaneously or require minimal intervention, while severe dysplasia may necessitate further evaluation and treatment to prevent progression to cervical precancerous lesions or cervical cancer. It is important to note that cervical dysplasia does not necessarily indicate the presence of cervical cancer, but it may increase the risk of developing it.
Symptoms of Cervical Dysplasia
Cervical dysplasia typically does not present obvious symptoms in its early stages, making regular cervical screening essential for early detection and treatment. However, as cervical dysplasia progresses to more severe stages, the following symptoms may occur:
-
Abnormal Vaginal Bleeding: This may include bleeding between menstrual periods, persistent bleeding after menstruation, postcoital bleeding, or painless vaginal bleeding.
-
Abnormal Vaginal Discharge: An increase in vaginal discharge may occur, potentially accompanied by a foul odor or blood.
-
Pelvic Pain: Discomfort or pain may be felt in the lower abdomen or pelvic area.
-
Dyspareunia: Discomfort or pain during sexual intercourse may also be experienced.
These symptoms are not exclusive to cervical dysplasia and may relate to other gynecological conditions. If any of these symptoms are experienced or if there are concerns, it is advisable to consult a gynecologist for evaluation and diagnosis.
Risk Factors for Cervical Dysplasia
-
Human Papillomavirus (HPV) Infection: Persistent HPV infection is the primary risk factor for cervical dysplasia.
-
Early Onset of Sexual Activity: Engaging in sexual activity at a younger age increases the likelihood of HPV infection.
-
Multiple Sexual Partners: Having multiple sexual partners raises the risk of contracting HPV.
-
Immunocompromised Conditions: Individuals with compromised immune systems may be more susceptible to HPV infection and the development of cervical dysplasia.
-
Smoking: Smoking is associated with an increased risk of cervical dysplasia.
Who Requires Loop Electrosurgical Excision Procedure (LEEP)?
-
The treatment approach for cervical dysplasia varies based on the type, severity, and individual circumstances. LEEP is particularly effective for addressing the following conditions:
-
Initial Assessment: LEEP may be utilized for further evaluation and diagnosis when cervical cytology shows highly abnormal or suspected cancerous cells.
-
Cervical Intraepithelial Neoplasia (CIN): CIN is an early form of cervical dysplasia detectable through Pap smear or cervical biopsy. If diagnosed with high-grade CIN (CIN 2 or CIN 3), a physician may recommend LEEP to excise the abnormal tissue.
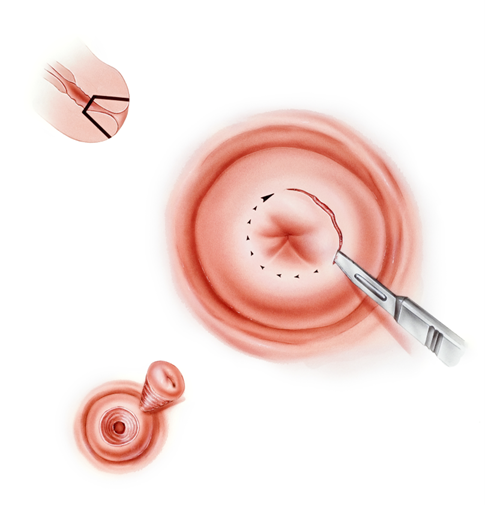
Procedure for Loop Electrosurgical Excision (LEEP)
-
Anesthesia: The procedure is performed under monitored anesthesia care and local anesthesia to ensure patient comfort, with an anesthesiologist supervising the process for safety.
-
Excision of Abnormal Tissue: The physician will use an electrosurgical loop to excise the abnormal tissue from the cervix. This loop utilizes high-frequency electrical current to cut and coagulate the abnormal cells, being carefully maneuvered to the area requiring excision.
-
Hemostasis: After removing the abnormal tissue, the physician will employ the electrosurgical loop or other methods to control bleeding, potentially utilizing electrocautery or other hemostatic techniques.
-
Tissue Examination: The excised tissue will be sent to the pathology laboratory for further examination to determine the presence of malignancy or other abnormalities, aiding in the decision for appropriate treatment.
Before the Procedure
-
Patients may be instructed to discontinue specific medications or follow dietary restrictions, particularly regarding anticoagulants or non-steroidal anti-inflammatory drugs (NSAIDs).
-
Patients should inform their physician of any wounds or ulcers in the genital area and avoid examinations during menstrual periods. If a patient is currently pregnant or suspects pregnancy, they should notify their physician.
-
Fasting instructions typically require patients to refrain from food intake for six hours before the procedure, with only small amounts of clear fluids allowed until two hours prior. Any prescribed preoperative medications should be taken as directed.
-
The physician will explain the rationale, process, and potential complications of the procedure, after which the patient may sign a consent form.
After the Procedure
-
Vaginal bleeding may occur for 7 to 10 days post-surgery, with mild abdominal discomfort possibly lasting two to three weeks.
-
Light vaginal bleeding is normal; however, patients should contact their physician if bleeding is excessive or prolonged. It is advisable to use pads instead of tampons to facilitate monitoring of blood loss.
-
Patients should avoid sexual intercourse, swimming, and the use of tampons for six weeks post-surgery to reduce the risk of infection.
-
Pain relievers and anti-inflammatory medications may be necessary as recommended by the physician.
-
Regular follow-up cervical cytology exams are essential; patients should adhere to their physician's recommendations for follow-up visits.
Follow-Up and Recovery
-
Patients may resume regular bathing.
-
Heavy lifting and vigorous exercise should be avoided for four to six weeks.
-
It is advisable to refrain from sexual activity for a few days post-examination to minimize the risk of infection and discomfort.
-
Common postoperative symptoms, such as headache, dizziness, nausea, or inflammation at the intravenous site, should resolve within a few days. Pain relievers may be taken as needed, and patients should prioritize rest after the procedure.
-
Patients should wait until the effects of anesthesia and sedation have worn off before resuming eating to prevent choking.
-
Alcohol consumption, operating heavy machinery, or driving is not advisable on the day of the procedure to prevent accidents. Patients should also refrain from signing any legal documents for 24 hours post-surgery.
-
Patients may leave the facility once the effects of anesthesia have dissipated but must be accompanied by an adult.
-
Contact your primary physician immediately if you experience any of the following symptoms: excessive vaginal bleeding, foul-smelling discharge, worsening abdominal pain (pelvic cramping), abdominal distension, chills, fever (temperature exceeding 38°C or 100°F), or any other abnormal conditions.
References
National Cancer Institute (US). Cervical Dysplasia - NCI Dictionary of Cancer Terms. Available at : https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cervical-dysplasia
Centre for Health Protection. Available at : https://www.chp.gov.hk/files/pdf/consensus_statement_on_the_use_of_hpv_vaccine_in_prevention_of_cervical_cancer.pdf
CDC. Cervical Cancer. Available at : https://www.cdc.gov/cervical-cancer/index.html

 3405 8288
3405 8288
